When small is big: MR safety for pediatric patients
March 16, 2021
By Tobias Gilk
MR safety is important for all patients, but it carries additional weight for our most vulnerable. As compared to MR safety for all patients, MR safety in pediatric environments is all the more emphasized, in part, because the most prominent MR accident in the United States — an accident that occurred 20 years ago this year — resulted in the death of a six-year-old boy. The weight of such a tragedy is simply that much more when the victim is a child.
Not only are public-perception consequences greater, but pediatric patients all bring unique and additional risk factors to MR imaging. Often children are less able to participate in their own pre-MR screening for risks or contraindications. Pediatric patients often require sedation or anesthesia in order to tolerate exams, and anesthesia both carries its own risks and can sometimes obscure native MR risks, too. And children with congenital and/or serious illnesses may need recurring MR scans throughout their developmental years, meaning that the risks are repeated, over and over. As a patient population, in several regards, children can add risk in MR.
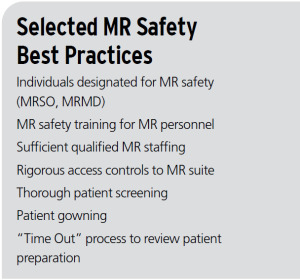
To be clear, MR is a profoundly safe study type, and injuries almost never occur because of malfunctions with the hardware. The accidents that do happen, however, are almost always because of poor decision-making at the point of care, and a failure to properly respect the real risks and hazards that do exist in MR imaging. Said another way, MR injuries are almost 100% preventable, so structured best practices and vigilance are the best tools for MR patient safety.
Unlike conventional X-ray-based modalities that have reams of state regulations, standards, and professional responsibility programs like “Image Gently” to guide pediatric radiation safety, MR providers are largely left to forge their own path for MR safety. There have been no formal “MR Safely” pledges as there are with the “Image Wisely” and “Image Gently” campaigns, and little in the way of fixed sets of best practices required for MR provider licensure or accreditation (despite accreditation entities’ near-universal marketing of “quality and safety” as the expected outcome of accreditation). In this regard, Katherine Bushur, the Advanced Modality supervisor for Children’s Hospital Colorado, acknowledges that “MR is behind the curve,” and MR patient safety — in general — doesn’t benefit from the regulatory, accreditation, or industry standards that ionizing radiation safety does.
Pediatric MR providers have emerged as one of the best “proving grounds” of MR safety best practices. This involves identifying effective best practice standards, and then a process of adoption and adaptation to where the practices and specific workflows are integrated. “It’s not copy and paste,” offers Bushur. “Every site is very different, and what works for us and what works for another children’s facility might be two entirely different processes, depending on what their workflows are.”
Bushur’s statements highlight a truth about safety practices, in general, and MR safety, in particular: they typically need to be translated from aspirational standard guidance to practical implementation, and that translation process requires thought and care to enable consistent and effective outcomes. Even beginning with widely respected standards, such as the ACR Manual on MR Safety, the “devil is in the details”, and a brilliant standard that is poorly integrated will not be expected to produce reliable results.
As for why pediatric MR providers are willing to put in this additional work (and are often regarded as more committed to MR safety), Bushur believes, “all patients are important, but I feel pediatric patients have a special place in people’s hearts and you take extra care because you’re not only treating the patient, but you’re also treating their family. It’s not just one little human, it’s the whole family that you’re taking care of when you take care of that patient.” In short, the stakes are higher. Based on reports from her techs who also take PRN work in general hospitals and imaging centers, “MR safety really isn’t taken to the level that we take it in the pediatric world.”
For this year, 2021, the anniversary of the MR death of Michael Colombini and a year dedicated to reflecting on MR safety, little could be more appropriate than to emulate the care and effort that children’s hospitals put into MR safety.
About the author: Tobias Gilk is an architect with RAD-Planning, and founded his own consulting firm, Gilk Radiology Consultants. He is both certified MRSO and MRSE, and is a board member and former chair of the American Board of Magnetic Resonance Safety (ABMRS).
MR safety is important for all patients, but it carries additional weight for our most vulnerable. As compared to MR safety for all patients, MR safety in pediatric environments is all the more emphasized, in part, because the most prominent MR accident in the United States — an accident that occurred 20 years ago this year — resulted in the death of a six-year-old boy. The weight of such a tragedy is simply that much more when the victim is a child.
Not only are public-perception consequences greater, but pediatric patients all bring unique and additional risk factors to MR imaging. Often children are less able to participate in their own pre-MR screening for risks or contraindications. Pediatric patients often require sedation or anesthesia in order to tolerate exams, and anesthesia both carries its own risks and can sometimes obscure native MR risks, too. And children with congenital and/or serious illnesses may need recurring MR scans throughout their developmental years, meaning that the risks are repeated, over and over. As a patient population, in several regards, children can add risk in MR.
To be clear, MR is a profoundly safe study type, and injuries almost never occur because of malfunctions with the hardware. The accidents that do happen, however, are almost always because of poor decision-making at the point of care, and a failure to properly respect the real risks and hazards that do exist in MR imaging. Said another way, MR injuries are almost 100% preventable, so structured best practices and vigilance are the best tools for MR patient safety.
Unlike conventional X-ray-based modalities that have reams of state regulations, standards, and professional responsibility programs like “Image Gently” to guide pediatric radiation safety, MR providers are largely left to forge their own path for MR safety. There have been no formal “MR Safely” pledges as there are with the “Image Wisely” and “Image Gently” campaigns, and little in the way of fixed sets of best practices required for MR provider licensure or accreditation (despite accreditation entities’ near-universal marketing of “quality and safety” as the expected outcome of accreditation). In this regard, Katherine Bushur, the Advanced Modality supervisor for Children’s Hospital Colorado, acknowledges that “MR is behind the curve,” and MR patient safety — in general — doesn’t benefit from the regulatory, accreditation, or industry standards that ionizing radiation safety does.
Pediatric MR providers have emerged as one of the best “proving grounds” of MR safety best practices. This involves identifying effective best practice standards, and then a process of adoption and adaptation to where the practices and specific workflows are integrated. “It’s not copy and paste,” offers Bushur. “Every site is very different, and what works for us and what works for another children’s facility might be two entirely different processes, depending on what their workflows are.”
Bushur’s statements highlight a truth about safety practices, in general, and MR safety, in particular: they typically need to be translated from aspirational standard guidance to practical implementation, and that translation process requires thought and care to enable consistent and effective outcomes. Even beginning with widely respected standards, such as the ACR Manual on MR Safety, the “devil is in the details”, and a brilliant standard that is poorly integrated will not be expected to produce reliable results.
As for why pediatric MR providers are willing to put in this additional work (and are often regarded as more committed to MR safety), Bushur believes, “all patients are important, but I feel pediatric patients have a special place in people’s hearts and you take extra care because you’re not only treating the patient, but you’re also treating their family. It’s not just one little human, it’s the whole family that you’re taking care of when you take care of that patient.” In short, the stakes are higher. Based on reports from her techs who also take PRN work in general hospitals and imaging centers, “MR safety really isn’t taken to the level that we take it in the pediatric world.”
For this year, 2021, the anniversary of the MR death of Michael Colombini and a year dedicated to reflecting on MR safety, little could be more appropriate than to emulate the care and effort that children’s hospitals put into MR safety.
About the author: Tobias Gilk is an architect with RAD-Planning, and founded his own consulting firm, Gilk Radiology Consultants. He is both certified MRSO and MRSE, and is a board member and former chair of the American Board of Magnetic Resonance Safety (ABMRS).