The latest news in defibrillators, patient monitoring and biomedical testing equipment
May 16, 2017
By James Laskaris and Julie Andrews, MD Buyline Analysts
Patient safety is always paramount in defibrillators, patient monitoring and biomedical testing equipment, but cost is always a factor.
Latest innovations in Defibrillators
The 2015 American Heart Association (AHA) Guidelines Update for advanced cardiac life support (ACLS) showed that a low end-tidal carbon dioxide (EtCO2) level in intubated patients was linked to a very low success rate for resuscitation. As a result, the ability to monitor EtCO2 during resuscitation efforts became a priority.
In response to this, all major defibrillator manufacturers have now added the ability to monitor EtCO2 to their manual equipment for both the acute care and EMS settings. The health care team can now assess the EtCO2 along with other vital signs during resuscitation and adjust the plan of care in real time.
The emphasis in any level of CPR training, from community-based to advanced, is on the rescuer performing high-quality CPR. Manufacturers have begun incorporating software into their professional devices that gives immediate feedback to the rescuer regarding the quality of compressions. If an automatic external defibrillator (AED) is in use, the feedback may be as simple as a digital message that reads “Push Harder” or “Good Compressions” or a visual meter that gives color feedback as compressions are performed.
Software is also available for manual defibrillators that can provide feedback during resuscitative efforts, and provide information that can be directly transferred to the electronic medical record (EMR) after the event. This can allow for vital quality review for the resuscitation team, and real-time accurate documentation in the patient’s medical record. This real-time documentation not only has an impact on the patient’s plan of care, but also on hospital coding and billing information.
Defibrillators, both manual and automated, use biphasic waveforms that come in three different forms: biphasic truncated; rectilinear biphasic; and pulsed biphasic. They all deliver peak energy at the same programmed settings, but differ in how they adjust energy output in relation to physical impedance. Mounting evidence shows a greater effectiveness for the biphasic truncated and rectilinear biphasic over that of the pulsed biphasic waveform. This information should be considered when purchasing either automated or manual defibrillation devices.
AEDs have become commonplace and an expectation in public venues such as sports arenas, airports and even on airplanes. First approved by the FDA in the 1990s, AED training became a part of the American Red Cross basic CPR course in 1999.
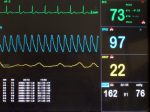
Latest innovations in patient monitoring
The latest trends in patient monitoring could be categorized in the areas of function and communication.
In the past, each patient care area would have specific patient monitoring parameters, and with that came a specific physical monitor. Today’s trend is for one physical monitor to be able to perform in a variety of patient care areas and even “follow” the patient throughout the hospital stay. In order to do this, patient monitoring manufacturers are being challenged to create the appropriate software for the monitor, and the physical configuration of the monitor must now come into play. The large, heavy, stationary monitor so often associated with the high-acuity patient care area, such as the ED, OR or ICU, must now be streamlined to also work as monitors in the sub-acute or medical/surgical patient care areas. These monitors are also expected to now perform as a transport monitor, and move with the patient between physical locations of care. This has motivated the leading manufacturers to streamline their products in both dimensions, weight and functionality.
As one patient monitor now becomes able to perform numerous functions, communicating this information to a central source, and eventually to the EMR, is essential. Real-time data transfer of patient information is essential in the ability of the health care team to access the information and plan care accordingly. As mobile devices become a more integral part of a care team’s ability to communicate with each other, the monitor must be able to obtain, store and accurately transfer data to a variety of devices.
Testing equipment
Biomedical test equipment represents a considerable investment. Costs can range from a couple of hundred dollars for simple volt meters to $10,000 to $20,000 or more for X-ray and laser test equipment. This does not even include the calibration costs that occur every year.
But as with any capital outlay question is what are you getting for your investment. Though the cost of test equipment has risen considerably in recent years, users have seen key advancements. These have translated to speed and cost savings.
Each year the U.S. health care industry will spend more than $14 billion for providing service on medical technology. This accounts for 3 to 7 percent of the original price per year (IT accounts for up to 20 percent per year). Although small in comparison to a facility’s overall labor costs (50 percent) or even what a hospital spends on consumables (15 to 20 percent), service on medical technology adds millions to running a hospital. With margins being squeezed harder than ever, providers are always looking for ways to improve care and lower costs.
One thing to consider when budgeting for test equipment is the cost of in-house service versus a vendor. Including benefits, in-house biomed staff makes $40 to $80 per hour. The vendor’s hourly labor costs typically start at $150 per hour based on time and materials charges. With this in mind, an upfront investment in test equipment will allow for long-term savings, especially if they have trained staff available.
In addition to direct savings, new systems have advanced considerably over the years. Historically, each performance test had to be performed separately and manually documented. This new generation of systems is capable of performing multiple tests simultaneously and documenting the results. This has allowed clinical engineering departments to further lower labor costs while performing key documentation to satisfy Joint Commission requirements.
About the authors: James Laskaris is a senior emerging technology analyst at MD Buyline and serves as the primary analyst of high-end operating room technology. He also covers issues related to the legislative and reimbursement effect on health care and authors a bimonthly “Issues that Matter” publication.
Julie Andrews is a clinical analyst at MD Buyline in the areas of critical care, nursing and patient monitoring, and has more than 20 years of experience as a registered nurse, nursing supervisor, clinical coordinator and clinical educator for ICU and telemetry.
Patient safety is always paramount in defibrillators, patient monitoring and biomedical testing equipment, but cost is always a factor.
Latest innovations in Defibrillators
The 2015 American Heart Association (AHA) Guidelines Update for advanced cardiac life support (ACLS) showed that a low end-tidal carbon dioxide (EtCO2) level in intubated patients was linked to a very low success rate for resuscitation. As a result, the ability to monitor EtCO2 during resuscitation efforts became a priority.
In response to this, all major defibrillator manufacturers have now added the ability to monitor EtCO2 to their manual equipment for both the acute care and EMS settings. The health care team can now assess the EtCO2 along with other vital signs during resuscitation and adjust the plan of care in real time.
The emphasis in any level of CPR training, from community-based to advanced, is on the rescuer performing high-quality CPR. Manufacturers have begun incorporating software into their professional devices that gives immediate feedback to the rescuer regarding the quality of compressions. If an automatic external defibrillator (AED) is in use, the feedback may be as simple as a digital message that reads “Push Harder” or “Good Compressions” or a visual meter that gives color feedback as compressions are performed.
Software is also available for manual defibrillators that can provide feedback during resuscitative efforts, and provide information that can be directly transferred to the electronic medical record (EMR) after the event. This can allow for vital quality review for the resuscitation team, and real-time accurate documentation in the patient’s medical record. This real-time documentation not only has an impact on the patient’s plan of care, but also on hospital coding and billing information.
Defibrillators, both manual and automated, use biphasic waveforms that come in three different forms: biphasic truncated; rectilinear biphasic; and pulsed biphasic. They all deliver peak energy at the same programmed settings, but differ in how they adjust energy output in relation to physical impedance. Mounting evidence shows a greater effectiveness for the biphasic truncated and rectilinear biphasic over that of the pulsed biphasic waveform. This information should be considered when purchasing either automated or manual defibrillation devices.
AEDs have become commonplace and an expectation in public venues such as sports arenas, airports and even on airplanes. First approved by the FDA in the 1990s, AED training became a part of the American Red Cross basic CPR course in 1999.
Latest innovations in patient monitoring
The latest trends in patient monitoring could be categorized in the areas of function and communication.
In the past, each patient care area would have specific patient monitoring parameters, and with that came a specific physical monitor. Today’s trend is for one physical monitor to be able to perform in a variety of patient care areas and even “follow” the patient throughout the hospital stay. In order to do this, patient monitoring manufacturers are being challenged to create the appropriate software for the monitor, and the physical configuration of the monitor must now come into play. The large, heavy, stationary monitor so often associated with the high-acuity patient care area, such as the ED, OR or ICU, must now be streamlined to also work as monitors in the sub-acute or medical/surgical patient care areas. These monitors are also expected to now perform as a transport monitor, and move with the patient between physical locations of care. This has motivated the leading manufacturers to streamline their products in both dimensions, weight and functionality.
As one patient monitor now becomes able to perform numerous functions, communicating this information to a central source, and eventually to the EMR, is essential. Real-time data transfer of patient information is essential in the ability of the health care team to access the information and plan care accordingly. As mobile devices become a more integral part of a care team’s ability to communicate with each other, the monitor must be able to obtain, store and accurately transfer data to a variety of devices.
Testing equipment
Biomedical test equipment represents a considerable investment. Costs can range from a couple of hundred dollars for simple volt meters to $10,000 to $20,000 or more for X-ray and laser test equipment. This does not even include the calibration costs that occur every year.
But as with any capital outlay question is what are you getting for your investment. Though the cost of test equipment has risen considerably in recent years, users have seen key advancements. These have translated to speed and cost savings.
Each year the U.S. health care industry will spend more than $14 billion for providing service on medical technology. This accounts for 3 to 7 percent of the original price per year (IT accounts for up to 20 percent per year). Although small in comparison to a facility’s overall labor costs (50 percent) or even what a hospital spends on consumables (15 to 20 percent), service on medical technology adds millions to running a hospital. With margins being squeezed harder than ever, providers are always looking for ways to improve care and lower costs.
One thing to consider when budgeting for test equipment is the cost of in-house service versus a vendor. Including benefits, in-house biomed staff makes $40 to $80 per hour. The vendor’s hourly labor costs typically start at $150 per hour based on time and materials charges. With this in mind, an upfront investment in test equipment will allow for long-term savings, especially if they have trained staff available.
In addition to direct savings, new systems have advanced considerably over the years. Historically, each performance test had to be performed separately and manually documented. This new generation of systems is capable of performing multiple tests simultaneously and documenting the results. This has allowed clinical engineering departments to further lower labor costs while performing key documentation to satisfy Joint Commission requirements.
About the authors: James Laskaris is a senior emerging technology analyst at MD Buyline and serves as the primary analyst of high-end operating room technology. He also covers issues related to the legislative and reimbursement effect on health care and authors a bimonthly “Issues that Matter” publication.
Julie Andrews is a clinical analyst at MD Buyline in the areas of critical care, nursing and patient monitoring, and has more than 20 years of experience as a registered nurse, nursing supervisor, clinical coordinator and clinical educator for ICU and telemetry.